What is a tendinopathy and what do I do about it?
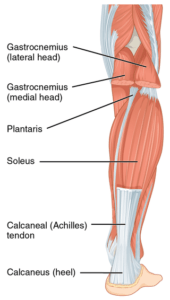
Tendon pain can develop in any tendon in the body. Foot, knee, hip, elbow, shoulder are all common areas for tendinopathies to occur. For example tennis elbow, jumpers knee, achilles issues are all tendinopathies. Tendons are a structure that connects muscles to our bones and they can become dysfunctional. Health professionals have called them lots of different names over the years like; tendonitis and tendinosis however, tendinopathy is now the correct term for these injuries.
There are usually 3 areas within a tendon that this pain can occur:
- Muscular tendon junction (this is where the tendon and muscle attach to each other)
- Mid- portion (middle of tendon)
- Insertion of tendon (where the tendon inserts into the bone)
Scans for tendinopathies
An ultrasound or MRI are the only scans that will allow you to see a tendon injury. It is important to note that a tendinopathy that is not painful can still show up on an ultrasound, ie tendinopathies that you have previously had can still be seen on the scan even if it is not painful anymore. This is normal and not something to worry about. Most of the time a good quality clinical assessment is of more value than imaging when it comes to tendons.
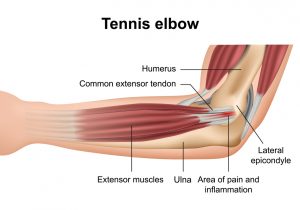 Tendon injuries typically occur when your tendon is unable to adapt to the load you expose it to, often if you train at an intensity that is too high and or there is not enough recovery time after activity before you train again. We also see tendon injuries when a person takes up a new activity or sport for the first time, exposing the tendon to new types of movements and loads or a heavy dose of an activity they don’t normally perform; eg elbow pain resulting from a twice per year gardening project.
Tendon injuries typically occur when your tendon is unable to adapt to the load you expose it to, often if you train at an intensity that is too high and or there is not enough recovery time after activity before you train again. We also see tendon injuries when a person takes up a new activity or sport for the first time, exposing the tendon to new types of movements and loads or a heavy dose of an activity they don’t normally perform; eg elbow pain resulting from a twice per year gardening project.
We all get some degree of muscle/tendon soreness or stiffness after a training session. What you’re feeling here is mild inflammation in the tendon in response to this loading. The tendon is repairing and becoming stronger. If during this phase we exercise too soon and too much, the inflammation can become excessive and the collagen fibres within the tendon can begin to disorganise and break down.
Staged and progressive loading is key to avoiding tendon injuries. Allow time for your body to recover before heading back to activity. If you’re not too sore complete a smaller session, or work parts of the body that aren’t sore. A well balanced diet low in sugar and carbohydrates, good hydration and 8 hours of regular sleep per night will all help to decrease inflammatory markers within the tendon.
I have tendon pain, should I rest?
No! In days gone past treatment and management of tendon pain was to rest and pain will get better. However, if you rest a tendon for too long it will adapt to the decrease in load and actually become weaker. This makes returning to activity particularly difficult. Although in some more serious cases of tendinopathy some rest from activity may be necessary. We are also often asked about cortisone injections for tendon injuries. While these can provide temporary pain relief there is research to suggest it actually weakens the tendon in the long run and is detrimental to overall recovery. However again in serious cases sometimes an injection is necessary for pain relief measures, we would always recommend a thorough assessment before booking the injection.
What exercises should I do?
Research throughout the 2000’s educated us to manage tendinopathies by loading them up with specific exercise dosages including isometric exercises and heavy slow resistance. Keeping in mind that if we do too much too soon the tendon cells inflame. This is where a good quality clinical examination comes into play. The examination will tell us what kind of exercise to do and how fast to progress someone.
It is often possible and safe to keep running/playing sport with mild symptoms while we progress through the rehab process. This is something we at GV Sportscare endeavour to do individually for the client as we understand how important physical activity is.
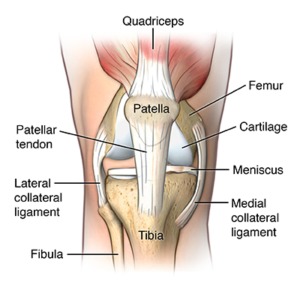
Podiatrists are highly skilled at treating tendon issues within the foot and achilles, while physiotherapists are experts in the rehab of tendon injuries in the knee (jumpers knee), hip (often referred to as bursitis), elbow (tennis and golfer’s elbow), wrist and shoulder.
Take home messages:
- Don’t do too much too soon. A progressive staged loading program is the safest way to increase load.
- Incorporate rest days into your training.
- A well balanced diet, 8 hours sleep and hydration will go a long way to aiding recovery from a tendon injury.
- Doing nothing and resting the tendon is most definitely not the answer.
See also for further information:
Foot pain: https://www.podiatry.org.au/foot-health-resources/pain
Tennis elbow: https://choose.physio/your-body/elbow/tennis-elbow
Achilles tendinopathy: https://choose.physio/your-body/ankle/achilles-tendinopathy
Image sources:
Achilles: https://en.wikipedia.org/wiki/Achilles_tendon
Elbow: https://www.joionline.net/library/show/lateral_epicondylitis_tennis_elbow/
Knee: https://www.hopkinsmedicine.org/health/conditions-and-diseases/patellar-tendonitis-jumpers-knee
Tom Davey
Podiatrist Shepparton, GV Sportscare