ACL rupture, why bother with prehab?
-Sophie Woodhouse
Physiotherapist Shepparton
GV Sportscare
-Sophie Woodhouse
Physiotherapist Shepparton
GV Sportscare

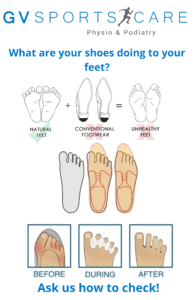
Tom achieves this via foot/leg strength, movement/mobility and footwear selection.
👞
Everyone needs natural foot shape and function to move pain free. Certain features in most modern shoes prevent the foot from functioning as it should.
👣
Building foot and leg strength, increasing mobility within the foot and avoiding particular shoe features can see a bunion return to normal over time.
⏰
Surgery for bunions is necessary in some cases. However, it is important to know that there are treatments and changes that can be utilised to fix or manage the bunion conservatively.
💉
Tom Davey
Podiatrist Shepparton, GV Sportscare
Low back pain can be frightening especially when your pain is severe or you are experiencing it for the first time. The pain may feel intense and you may begin to worry there is something sinister going on. This is where your healthcare professionals should be utilised. Our Shepparton physiotherapists are well trained in recognising what is low back pain and what needs further investigation. Around 90-95% of low back pain is benign and usually related to either muscle or ligamentous tissue (Lateef & Patel., 2009).
It can be tempting to rush straight to an x-ray or MRI or another form of scan. However it is often unnecessary. In fact getting an MRI in the first 6 weeks of onset of your low back pain can actually be detrimental to your long term recovery.
(From research into this area the following recommendations are made to both the medical and allied health professions)
(Webster et. al., 2010; Webster et. al., 2014)
These are important things to consider as not only is a scan not essential to treat your low back pain it can actually reduce your overall recovery.
A lumbar MRI needs careful explanation to avoid the danger of false positives. Your physio can explain your scan as often things that are reported on your scan have nothing to do with your pain at all and are found in individuals without pain. Around 57% of those 60 years and older who have no symptoms have an abnormal scan, disc bulge is a common finding (Baker et. al., 2014). In the younger age group of 20-39 year olds we see at least one disc bulge in the lumbar spine for those with no symptoms (Baker et. al, 2014). This highlights the fact that your scan needs to be read by your healthcare professional and explained so that you understand what is actually relevant to you and your pain experience.
To summarise, low back pain is a common phenomenon and your physiotherapist can assist you to understand the acute management including whether a scan is required or not. In many cases reassurance and education can save time, money and most importantly improve outcomes for the short and long term.
Australian Physio Association, choosing wisely.
Imaging for low back pain, American Academy of Family Physicians
References
Baker, A. D. (2014). Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects. A prospective investigation. In Classic Papers in Orthopaedics (pp. 245-247). Springer London.
Lateef, H., & Patel, D. (2009). What is the role of imaging in acute low back pain?. Current reviews in musculoskeletal medicine, 2(2), 69-73.
Webster, B. S., Choi, Y., Bauer, A. Z., Cifuentes, M., & Pransky, G. (2014). The cascade of medical services and associated longitudinal costs due to nonadherent magnetic resonance imaging for low back pain. Spine, 39(17), 1433.
Webster, Barbara S., and Manuel Cifuentes. “Relationship of early magnetic resonance imaging for work-related acute low back pain with disability and medical utilization outcomes.” Journal of occupational and environmental medicine 52, no. 9 (2010): 900-907.
Sophie Woodhouse
Physiotherapist Shepparton, GV Sportscare
