Achilles tendon pain
I have pain in my achilles tendon, should I rest it?

Tom Davey
Podiatrist Shepparton, GV Sportscare

Tom Davey
Podiatrist Shepparton, GV Sportscare
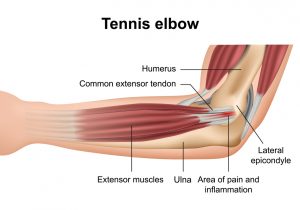
Tennis Elbow 🤔
Did you know that this condition is seen commonly in desk workers, golfers and weekend gardeners? 👩🌾👨💻🏌️♀️
The extensor muscles and tendon in the forearm can be overworked by repetitive wrist extension or gripping. You might notice pain when trying to lift the kettle, open doors, lifting moderate to heavy loads or after long days on the computer. This pain can radiate up into the bicep or tricep and all the way down into the wrist or the hand.
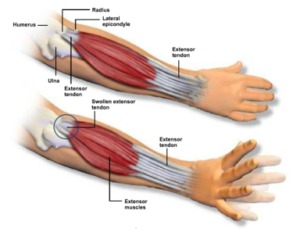
Our physiotherapist Sophie can give you the tools and education you need to avoid continual overload and get you going on exercises to strengthen the tendon.
Quick tip: ‘Don’t poke or rub the elbow when it is sore, tendon’s hate to be compressed and although it may feel like the right thing to do, you are continuing to aggravate the tendon!’ 🙅♀️


Image source: https://www.knoxorthopedic.com/f-s-t-cure-tennis-elbow-lat…/
Sophie Woodhouse
Physiotherapist Shepparton, GV Sportscare

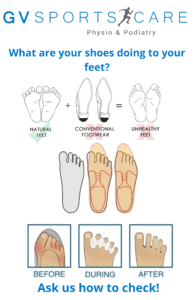
Tom achieves this via foot/leg strength, movement/mobility and footwear selection.
👞
Everyone needs natural foot shape and function to move pain free. Certain features in most modern shoes prevent the foot from functioning as it should.
👣
Building foot and leg strength, increasing mobility within the foot and avoiding particular shoe features can see a bunion return to normal over time.
⏰
Surgery for bunions is necessary in some cases. However, it is important to know that there are treatments and changes that can be utilised to fix or manage the bunion conservatively.
💉
Tom Davey
Podiatrist Shepparton, GV Sportscare
Ankle sprains are one of the most common injuries to occur. Women are at greater risk, as are children and adolescents and those that play indoor or court sports such as basketball or netball. This probably comes as no surprise, what may surprise you is how the management of these injuries has progressed away from the old ‘ice and rest’. At GV Sportscare our Shepparton Podiatrist and Physiotherapists are experts in ankle sprains, having worked on football teams, netball teams and closely with foot and ankle surgeons. Read on to learn about some of the myths behind ankle sprains!
 Most people are surprised to find that their physio or podiatrist is very keen to get them off crutches ASAP. In severe ankle sprains or suspected fractures, crutches are required, however in the mild to moderate ankle sprain crutches will actually slow down your recovery. Crutches reduce the weightbearing through the joint (which is a good thing if there is too much pain and damage). However in a mild to moderate injury it is unnecessary and will cause you to lose movement and strength, which you will need to work harder to regain as part of your rehab. Your Shepparton Physio or Podiatrist are able to assess your injury and guide you as to whether or not crutches are required and work with you to wean you off them!
Most people are surprised to find that their physio or podiatrist is very keen to get them off crutches ASAP. In severe ankle sprains or suspected fractures, crutches are required, however in the mild to moderate ankle sprain crutches will actually slow down your recovery. Crutches reduce the weightbearing through the joint (which is a good thing if there is too much pain and damage). However in a mild to moderate injury it is unnecessary and will cause you to lose movement and strength, which you will need to work harder to regain as part of your rehab. Your Shepparton Physio or Podiatrist are able to assess your injury and guide you as to whether or not crutches are required and work with you to wean you off them!
Podiatrists and Physios are well trained in assessing and treating ankle sprains and can refer you for any relevant scans such as x-ray and MRI, if required. We have specialist tests we can perform and provide you with taping or ankle supports on the spot, should you need them. We can also begin your rehab process of exercises from your very first session. This is very important as early movement and strength work can fasten your recovery or return to sport. So in summary within one physio or podiatry session we can diagnose or send for scans, tape or fit a brace or crutches (if necessary) and start you on exercises, all with the goal of return to activity or sport ASAP!
X-ray is used to clear fractures. Some fractures are too small to be picked up on x-ray and require a CT or MRI. This can include what we call an OCD (osteochondral defect), where a small piece of bone/cartilage has chipped off and can be sitting somewhere it shouldn’t. These often need to be removed as they can push and wear away on the cartilage where they shouldn’t.
X-ray is always used when the person is unable to weightbear as a precaution to check for fracture (we are actually required to x-ray if you cannot weightbear). This is even more important in the child or adolescent as they are more likely to fracture. This is because in children the bones aren’t fully fused as in adult bones and therefore the bones are more susceptible to fracture.

X-ray also can’t tell you how severe your ligamentous injury is. Sometimes you can see a syndesmosis injury (when the tibia and fibula have separated due to damage to the ligaments between them) on x-ray. However ligamentous injuries can often take much longer to recover from and have long lasting effects on your ankle stability.
 The sooner you can be seen by your Podiatrist or Physio the better. When we waste a few days with the wrong management you are slowing down your recovery. Most people think injuries are a time based recovery, ie I have sustained a grade one ankle sprain therefore I will be back to sport in 2 weeks. This is partly true, injuries require healing and that takes time. However from our point of view your return to sport or activity is mostly based on ticking off certain criteria. For example can you raise onto your toes, can you stand on one leg, can you hop, can you run, etc. If you can’t do these things it doesn’t matter if your two weeks has passed, you are still not ready to return to activity. We then base our rehab on what you can and can’t do and aim to progress you on as quickly as possible.
The sooner you can be seen by your Podiatrist or Physio the better. When we waste a few days with the wrong management you are slowing down your recovery. Most people think injuries are a time based recovery, ie I have sustained a grade one ankle sprain therefore I will be back to sport in 2 weeks. This is partly true, injuries require healing and that takes time. However from our point of view your return to sport or activity is mostly based on ticking off certain criteria. For example can you raise onto your toes, can you stand on one leg, can you hop, can you run, etc. If you can’t do these things it doesn’t matter if your two weeks has passed, you are still not ready to return to activity. We then base our rehab on what you can and can’t do and aim to progress you on as quickly as possible.
Icing is great to help numb the area and therefore relieve pain. However compression and elevation are far more important to help decrease your inflammation. Swelling in the ankle is particularly hard to get rid of due to gravity, as the fluid has no chance to escape the area. Compression helps to increase the pressure and essentially push the fluid out and elevation allows gravity to assist the swelling to move out of the area. There is actually very limited scientific research to prove that icing has much effect on swelling!

Swelling management: you can see the effects of a compression bandage and elevation on the swelling of this ankle.
 In the first 48-72 hours of your injury it is recommended to avoid anti inflammatories such as ibuprofen (Nurofen) and Voltaren. This is because the inflammation that occurs is your body’s response to injury and it actually brings special healing cells to the area that are beneficial for your recovery. This includes cells that remove debris and other cells that repair tissue. Therefore this early inflammation is actually a GOOD thing and taking anti inflammatories will be detrimental to this process (FYI this is true of any injury, not just ankle sprains).
In the first 48-72 hours of your injury it is recommended to avoid anti inflammatories such as ibuprofen (Nurofen) and Voltaren. This is because the inflammation that occurs is your body’s response to injury and it actually brings special healing cells to the area that are beneficial for your recovery. This includes cells that remove debris and other cells that repair tissue. Therefore this early inflammation is actually a GOOD thing and taking anti inflammatories will be detrimental to this process (FYI this is true of any injury, not just ankle sprains).
The issue is when inflammation persists and essentially the fluid takes up room within your ankle joints and this can cause pressure and therefore additional pain. This is where the above advice for compression and elevation is key and at some stage after the first few days you may need to begin anti inflammatories. This should always be guided by a health care professional as anti inflammatories can commonly cause stomach lining irritation, which is not something to ignore!
If you need help with pain relief it is recommended to speak with your pharmacist or local Shepparton GP, however most people tolerate paracetamol (Panadol) and this has no known negative effect on your healing.
You may have noticed that everyone bruises to a different degree. For example some people just have to scratch their leg firmly and will bruise while others need a decent hit to bruise. This is related to each person’s clotting and other genetic factors. It can also be related to certain medication for example blood thinners and anti inflammatories can increase the amount of bleeding around an area and therefore the amount fo bruising that comes out. Therefore the amount of bruising that is evident in some ankle sprains doesn’t necessarily mean it is more severe than other injuries where there is minimal bruising. We take into account many factors when diagnosing the severity of the injury, bruising is taken into consideration but there is no hard and fast rule here.

A severe ankle sprain: minimal dark bruising, mostly yellow.

Although when in pain this is what we feel like doing, there is good evidence that early movement will help you to return to normal quicker. When you have sustained a severe injury or you have a lot of swelling you will require periods where you need to elevate your ankle. However if you are able to walk and weightbear this will be helpful. This is where it is important to visit your local Shepparton podiatrist or physiotherapist so we can help you determine what level of rest is required!
 One of the biggest risk factors for future ankle sprain is previous ankle sprain. While those with mild ankle sprains will likely manage to get back to sport, the issue we commonly see is that the injury has caused a loss of range of motion, strength, balance or coordination on that side. Therefore you can understand how even though you have returned to sport that these deficiencies can result in subsequent ankle sprains and more time away from the sport that you love! With simple assessment and exercises we can get you on track to work on these deficiencies and therefore reduce your risk of future ankle injury!
One of the biggest risk factors for future ankle sprain is previous ankle sprain. While those with mild ankle sprains will likely manage to get back to sport, the issue we commonly see is that the injury has caused a loss of range of motion, strength, balance or coordination on that side. Therefore you can understand how even though you have returned to sport that these deficiencies can result in subsequent ankle sprains and more time away from the sport that you love! With simple assessment and exercises we can get you on track to work on these deficiencies and therefore reduce your risk of future ankle injury!
Both ankle bracing and taping are thought to be just as effective in preventing ankle sprains and are highly recommended for those who have had an ankle injury and are playing sports such as netball, football, basketball, soccer etc. While some are resistant to taping or bracing, when comparing this to lengthy periods out of action should another ankle sprain occur, we know what we would chose!
The advantages to ankle braces is that you aren’t reliant on the person taping your ankle to tape it correctly or risk of tape cuts or allergic responses to tape (which is more common than you think). If you are paying for your own tape, bracing is also a more economical option as once you have bought 4-5 rolls of tape you have paid for your ankle brace. However football and soccer boots are too narrow for ankle braces so taping is often the only option in these sports. If you wear ankle braces and you are buying new shoes we highly recommend taking your ankle braces with you as you often need 0.5-1 size larger to allow for the ankle brace. We would also advise checking with your Physio or Podiatrist before purchasing an ankle brace as many braces don’t have the metal ‘stays’ built in on the sides and this a crucial component of an ankle brace that will actually prevent injury.
As a netball or footballer you may be one of those people where ~2 sprains/season is a given and you are well versed in your management. We do recommend these are still assessed for a number of reasons:
-recurrent sprains can result in chronic ankle instability, at some stage ankle reconstruction may need to be considered so that you don’t cause irreversible cartilage damage which can lead to osteoarthritis in later life. As we have worked closely with foot and ankle orthopaedic surgeons we can help you decipher when it is time to consider a surgical opinion
-some ankle sprains can result in a ‘high ankle sprain’ which is an injury to the syndesmosis, the joint between to the tibia and fibula. This is a much more serious injury and requires a different management to the average ankle sprain. It can often require surgery to prevent serious ankle instability. Our Shepparton physio and podiatrist can easily screen for this injury with clinical tests
-refer to myth #8, we are experts in finding your deficiencies post injury and providing you with a rehab plan to address this to reduce your risk of re-injury.
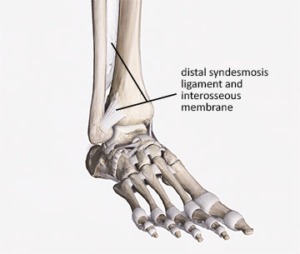
Distal syndesmosis joint = location of high ankle sprain.
Sophie Woodhouse
Physiotherapist Shepparton, GV Sportscare
Tom Davey
Podiatrist Shepparton, GV Sportscare

Image references:
X-ray: https://www.imageinterpretation.co.uk/ankle.php
Calf raise: https://www.popsugar.com.au/fitness/Ankle-Exercises-Do-Avoid-Sprains-Injuries-31086537?utm_medium=redirect&utm_campaign=US:AU&utm_source=www.google.com
Syndesmosis: https://www.academyofclinicalmassage.com/syndesmosis-sprains/
Ankle brace: https://www.djoglobal.com/products/donjoy/donjoy-stabilizing-pro-ankle-brace
Ankle sprain prevention: https://www.facebook.com/watch/?v=948001962331923
Watch our video introducing Shepparton’s Physio and Podiatry team, GV Sportscare and learn how we work together to get the best outcome for you!
Low back pain can be frightening especially when your pain is severe or you are experiencing it for the first time. The pain may feel intense and you may begin to worry there is something sinister going on. This is where your healthcare professionals should be utilised. Our Shepparton physiotherapists are well trained in recognising what is low back pain and what needs further investigation. Around 90-95% of low back pain is benign and usually related to either muscle or ligamentous tissue (Lateef & Patel., 2009).
It can be tempting to rush straight to an x-ray or MRI or another form of scan. However it is often unnecessary. In fact getting an MRI in the first 6 weeks of onset of your low back pain can actually be detrimental to your long term recovery.
(From research into this area the following recommendations are made to both the medical and allied health professions)
(Webster et. al., 2010; Webster et. al., 2014)
These are important things to consider as not only is a scan not essential to treat your low back pain it can actually reduce your overall recovery.
A lumbar MRI needs careful explanation to avoid the danger of false positives. Your physio can explain your scan as often things that are reported on your scan have nothing to do with your pain at all and are found in individuals without pain. Around 57% of those 60 years and older who have no symptoms have an abnormal scan, disc bulge is a common finding (Baker et. al., 2014). In the younger age group of 20-39 year olds we see at least one disc bulge in the lumbar spine for those with no symptoms (Baker et. al, 2014). This highlights the fact that your scan needs to be read by your healthcare professional and explained so that you understand what is actually relevant to you and your pain experience.
To summarise, low back pain is a common phenomenon and your physiotherapist can assist you to understand the acute management including whether a scan is required or not. In many cases reassurance and education can save time, money and most importantly improve outcomes for the short and long term.
Australian Physio Association, choosing wisely.
Imaging for low back pain, American Academy of Family Physicians
References
Baker, A. D. (2014). Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects. A prospective investigation. In Classic Papers in Orthopaedics (pp. 245-247). Springer London.
Lateef, H., & Patel, D. (2009). What is the role of imaging in acute low back pain?. Current reviews in musculoskeletal medicine, 2(2), 69-73.
Webster, B. S., Choi, Y., Bauer, A. Z., Cifuentes, M., & Pransky, G. (2014). The cascade of medical services and associated longitudinal costs due to nonadherent magnetic resonance imaging for low back pain. Spine, 39(17), 1433.
Webster, Barbara S., and Manuel Cifuentes. “Relationship of early magnetic resonance imaging for work-related acute low back pain with disability and medical utilization outcomes.” Journal of occupational and environmental medicine 52, no. 9 (2010): 900-907.
Sophie Woodhouse
Physiotherapist Shepparton, GV Sportscare
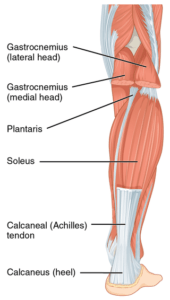
Tendon pain can develop in any tendon in the body. Foot, knee, hip, elbow, shoulder are all common areas for tendinopathies to occur. For example tennis elbow, jumpers knee, achilles issues are all tendinopathies. Tendons are a structure that connects muscles to our bones and they can become dysfunctional. Health professionals have called them lots of different names over the years like; tendonitis and tendinosis however, tendinopathy is now the correct term for these injuries.
There are usually 3 areas within a tendon that this pain can occur:
Scans for tendinopathies
An ultrasound or MRI are the only scans that will allow you to see a tendon injury. It is important to note that a tendinopathy that is not painful can still show up on an ultrasound, ie tendinopathies that you have previously had can still be seen on the scan even if it is not painful anymore. This is normal and not something to worry about. Most of the time a good quality clinical assessment is of more value than imaging when it comes to tendons.
 Tendon injuries typically occur when your tendon is unable to adapt to the load you expose it to, often if you train at an intensity that is too high and or there is not enough recovery time after activity before you train again. We also see tendon injuries when a person takes up a new activity or sport for the first time, exposing the tendon to new types of movements and loads or a heavy dose of an activity they don’t normally perform; eg elbow pain resulting from a twice per year gardening project.
Tendon injuries typically occur when your tendon is unable to adapt to the load you expose it to, often if you train at an intensity that is too high and or there is not enough recovery time after activity before you train again. We also see tendon injuries when a person takes up a new activity or sport for the first time, exposing the tendon to new types of movements and loads or a heavy dose of an activity they don’t normally perform; eg elbow pain resulting from a twice per year gardening project.
We all get some degree of muscle/tendon soreness or stiffness after a training session. What you’re feeling here is mild inflammation in the tendon in response to this loading. The tendon is repairing and becoming stronger. If during this phase we exercise too soon and too much, the inflammation can become excessive and the collagen fibres within the tendon can begin to disorganise and break down.
Staged and progressive loading is key to avoiding tendon injuries. Allow time for your body to recover before heading back to activity. If you’re not too sore complete a smaller session, or work parts of the body that aren’t sore. A well balanced diet low in sugar and carbohydrates, good hydration and 8 hours of regular sleep per night will all help to decrease inflammatory markers within the tendon.
I have tendon pain, should I rest?
No! In days gone past treatment and management of tendon pain was to rest and pain will get better. However, if you rest a tendon for too long it will adapt to the decrease in load and actually become weaker. This makes returning to activity particularly difficult. Although in some more serious cases of tendinopathy some rest from activity may be necessary. We are also often asked about cortisone injections for tendon injuries. While these can provide temporary pain relief there is research to suggest it actually weakens the tendon in the long run and is detrimental to overall recovery. However again in serious cases sometimes an injection is necessary for pain relief measures, we would always recommend a thorough assessment before booking the injection.
What exercises should I do?
Research throughout the 2000’s educated us to manage tendinopathies by loading them up with specific exercise dosages including isometric exercises and heavy slow resistance. Keeping in mind that if we do too much too soon the tendon cells inflame. This is where a good quality clinical examination comes into play. The examination will tell us what kind of exercise to do and how fast to progress someone.
It is often possible and safe to keep running/playing sport with mild symptoms while we progress through the rehab process. This is something we at GV Sportscare endeavour to do individually for the client as we understand how important physical activity is.
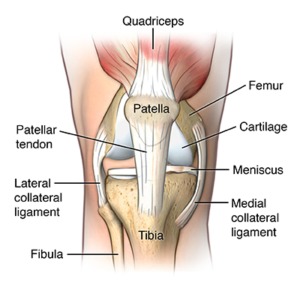
Podiatrists are highly skilled at treating tendon issues within the foot and achilles, while physiotherapists are experts in the rehab of tendon injuries in the knee (jumpers knee), hip (often referred to as bursitis), elbow (tennis and golfer’s elbow), wrist and shoulder.
Take home messages:
Foot pain: https://www.podiatry.org.au/foot-health-resources/pain
Tennis elbow: https://choose.physio/your-body/elbow/tennis-elbow
Achilles tendinopathy: https://choose.physio/your-body/ankle/achilles-tendinopathy
Image sources:
Achilles: https://en.wikipedia.org/wiki/Achilles_tendon
Elbow: https://www.joionline.net/library/show/lateral_epicondylitis_tennis_elbow/
Knee: https://www.hopkinsmedicine.org/health/conditions-and-diseases/patellar-tendonitis-jumpers-knee
Tom Davey
Podiatrist Shepparton, GV Sportscare
A common complaint we often hear is ‘I’ve got a headache, I know it’s coming from my neck’, but have you ever thought why neck issues can cause headaches? We call this a Cervicogenic headache, meaning headache originating from the cervical spine (the neck).
The main issue at play is the nerves that carry information from the upper 3 segments of the cervical spine (C1-3) converge on the same point in the brain that informs it of head pain. Due to the anatomy of the nerves the brain essentially is confused about where the pain is coming from and therefore neck pain is instead interpreted as a headache.
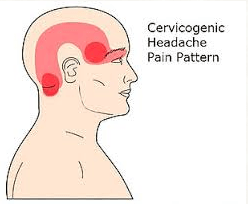 For some people this is one sided, for example their right neck joints and muscles will refer pain to the right side of the head causing a right sided headache. This is often reflected in the examination performed by the physiotherapist where the right side of the neck will be much more tender to touch than the left.
For some people this is one sided, for example their right neck joints and muscles will refer pain to the right side of the head causing a right sided headache. This is often reflected in the examination performed by the physiotherapist where the right side of the neck will be much more tender to touch than the left.
For people with cervicogenic headaches, physiotherapy can therefore be of great benefit as we can find the cause of the neck pain and work to release and strengthen the neck. Reducing the tension on the neck therefore reduces the neural input to the brain that signifies pain that is then interpreted as a headache. This includes a thorough assessment to identify what activities or postures are placing additional strain on your neck. For example some desk workers who spend long time sitting and use a mouse in their right hand will find that they fatigue the right side of their shoulder and neck muscles. The physiotherapist will then work to find strategies to reduce this tension via actions taken at work while also using soft tissue and mobilisation techniques, followed by a strengthening program.
It is also important to note that most headaches are multifactorial and other factors include hormonal, blood pressure, stress, mental health and medication. Each of these factors will need to be explored to varying levels in different people. This may involve consultation with other health professionals.
See also this blog by the Australian Physiotherapy Association for more information:
https://choose.physio/your-body/neck/neck-related-cervicogenic-headache
References:
Biondi, D. M. (2005). Cervicogenic headache: a review of diagnostic and treatment strategies. The Journal of the American Osteopathic Association, 105(4_suppl), 16S-22S.
Bogduk, N. (2001). Cervicogenic headache: anatomic basis and pathophysiologic mechanisms. Current pain and headache reports, 5(4), 382-386.
Image source: https://postpt.com/web/headaches-we-all-get-them-cherie-is-here-to-educate-us/
Sophie Woodhouse
Physiotherapist Shepparton, GV Sportscare
